Introduction to stress
The word ‘stress’ was first used in life science by Hans Selye in 1936. It is derived from the Latin word “stringere” which means “tight,” or “strained”. In the last few decades, research has demonstrated a correlation between stress and periodontal diseases. Our current knowledge of the etiopathogenesis of periodontal diseases indicates that periodontitis is a multifactorial disease in which the host factors and the environmental factors play an important role 1. Though bacterial plaque is considered as the primary etiology of periodontal diseases, other factors like smoking, alcohol consumption, systemic diseases like diabetes, genetic factors, and stress can influence the disease progression to a considerable extent. The associations between stress levels and periodontal disease have been examined in several studies 2-5. Stress influences the host defense system by exerting an immunosuppressive effect, thereby leading to increased vulnerability to disease 6, 7. Genco et al. (1999) 8 suggested that psychosocial stress is a significant risk indicator for more severe periodontal disease, along with smoking and the presence of Tannerella forsythia and Porphyromonas gingivalis. In the following discussion, we shall study different aspects of stress and its direct and indirect effects on periodontal disease progression.
Definitions
A stressor is any stimulus, situation or circumstance with the potential to induce stress reactions 9. Some of the well-accepted definitions of stress are as follows,
- Stress is a state of physiological or psychological strain caused by adverse stimuli, physical, mental, or emotional, internal or external, that tend to disturb the functioning of an organism and which the organism naturally desires to avoid 10.
- An inharmonious fit between the person and the environment, one in which the person’s resources are taxed or exceeded, forcing the person to struggle, usually in complex ways to cope 11.
- Stress is defined as physiological and metabological perturbations caused by various aggressive agents and the psychophysiological response of an organism facing the perception of a challenge or a threat 12.
The psychological stressors may result from major stressful life events or from minor daily stressors, resulting from day to day problems. The psychological stress is also a result of ………… Contents available in the book……………….. Contents available in the book……………….. Contents available in the book……………….. Contents available in the book………
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
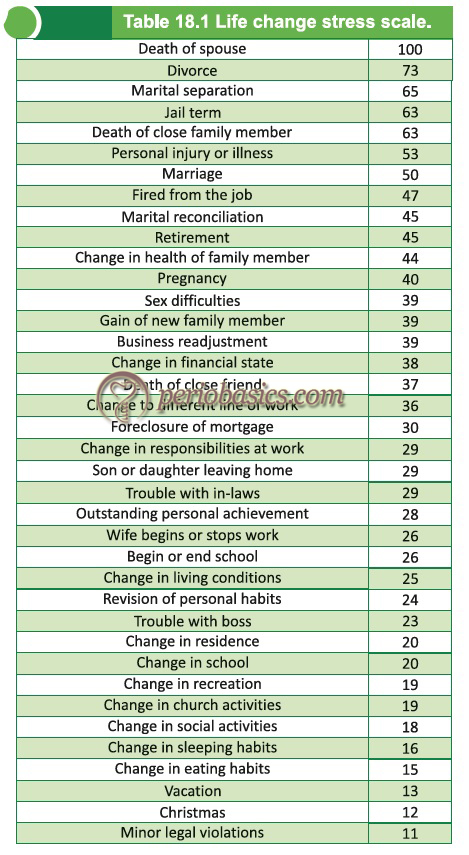
Scoring of psychological stressors
Although stress levels for a particular event vary from person to person and it is very difficult to generalize the level of stress that different individuals take for a particular event, Holmes in 1967 developed a scale to measure stress in terms of life changes. The life events on the scale were ranked from most stressful to least stressful as shown in the following table,
Evidence for relationship of stress and periodontal disease progression
The pioneers who suggested psychological stress might play a role as an etiological agent of periodontal disease were Dean and Dean (1945) 14 and Schluger (1949) 15. Many investigations have shown that psychological stress can downregulate the cellular immune response 13, 16-18. Many Cross-sectional studies 19-21 highlighted a clear-cut correlation between the progressive course of periodontal disease and the psychosocial stress status of patients. Necrotizing ulcerative gingivitis and periodontitis (NUG and NUP) are the most frequently associated and well documented periodontal conditions associated with psychological stress 22.
In a study, Genco (1995) analyzed the data from 1400 people of 25-75 years of age to find out if stress, distress, and poor coping behaviors are risk factors of periodontitis. It was concluded that people with financial stress had more severe periodontal disease 23. In another study, Shannon et al. (1969) 24 investigated the possible relationship between stress and ANUG, as measured by the urinary steroid excretion rate, in 478 males being screened in military duty. Results showed that patients with ANUG had increased corticosteroid activity in urine. The view that stress is an etiologic factor in ANUG is further strengthened by adrenocortical activity.
A prospective observational study done on students, assessing the clinical signs of periodontal disease (such as gingival bleeding on probing) and diagnosed gingivitis showed that severe deterioration in gingival health from baseline levels was observed during the period of academic examinations in cases as compared to control group 25. On the contrary, one study failed to confirm the link between the type of periodontal disease and psychological stressors that included depression, anxiety, perceived stress and loneliness, and dental plaque as the major dependent variable 22.
The stress pathway
Stress can be classified into acute and chronic types, depending on its time duration. Acute stress lasts for a period of minutes to hours, whereas chronic stress persists for several hours, days, weeks or even months 26. Acute stress is often a challenge such as due to infection, which prepares the immune system for immediate response. But chronic stress may influence inflammatory processes, leading to the development of systemic or local diseases such as rheumatoid arthritis 27, diabetes 28, cardiovascular diseases 29 or periodontal diseases 30. Let us try to understand the effects of stressful events on central nervous system and the immune system.
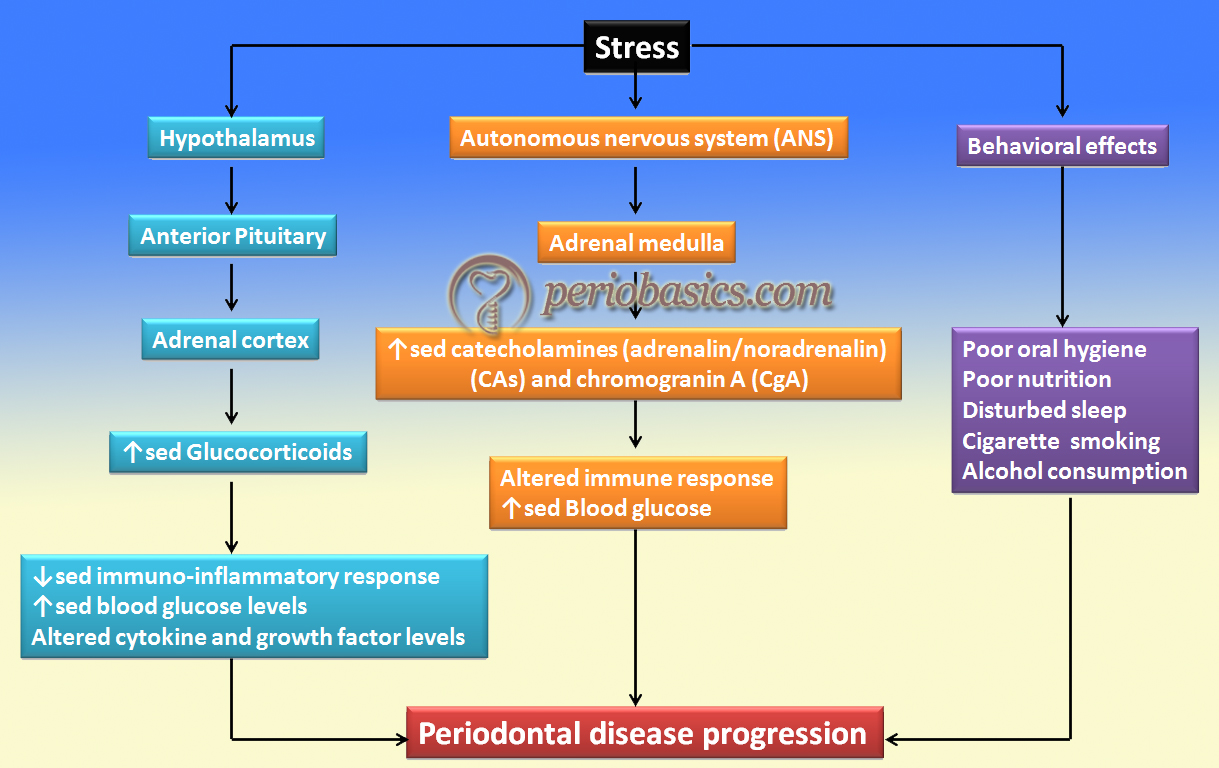
First of all, it is important to understand that all the events that occur under stress are subjected to promote the protection of the organism 31. Two major pathway systems are involved in the stress pathway: the hypothalamic-pituitary-adrenal (HPA) axis and the systemic/adrenomedullary sympathetic nervous system (SNS). Under the influence of a stressful event, the hypothalamus-pituitary-adrenal (HPA) axis is stimulated by the anterior hypothalamus, leading to the secretion of corticotropin-releasing hormone (CRH) and arginine vasopressin that act on the pituitary gland. In turn, the adrenocorticotrophic hormone is secreted by the pituitary gland, which acts on the ………… Contents available in the book……………….. Contents available in the book……………….. Contents available in the book……………….. Contents available in the book………
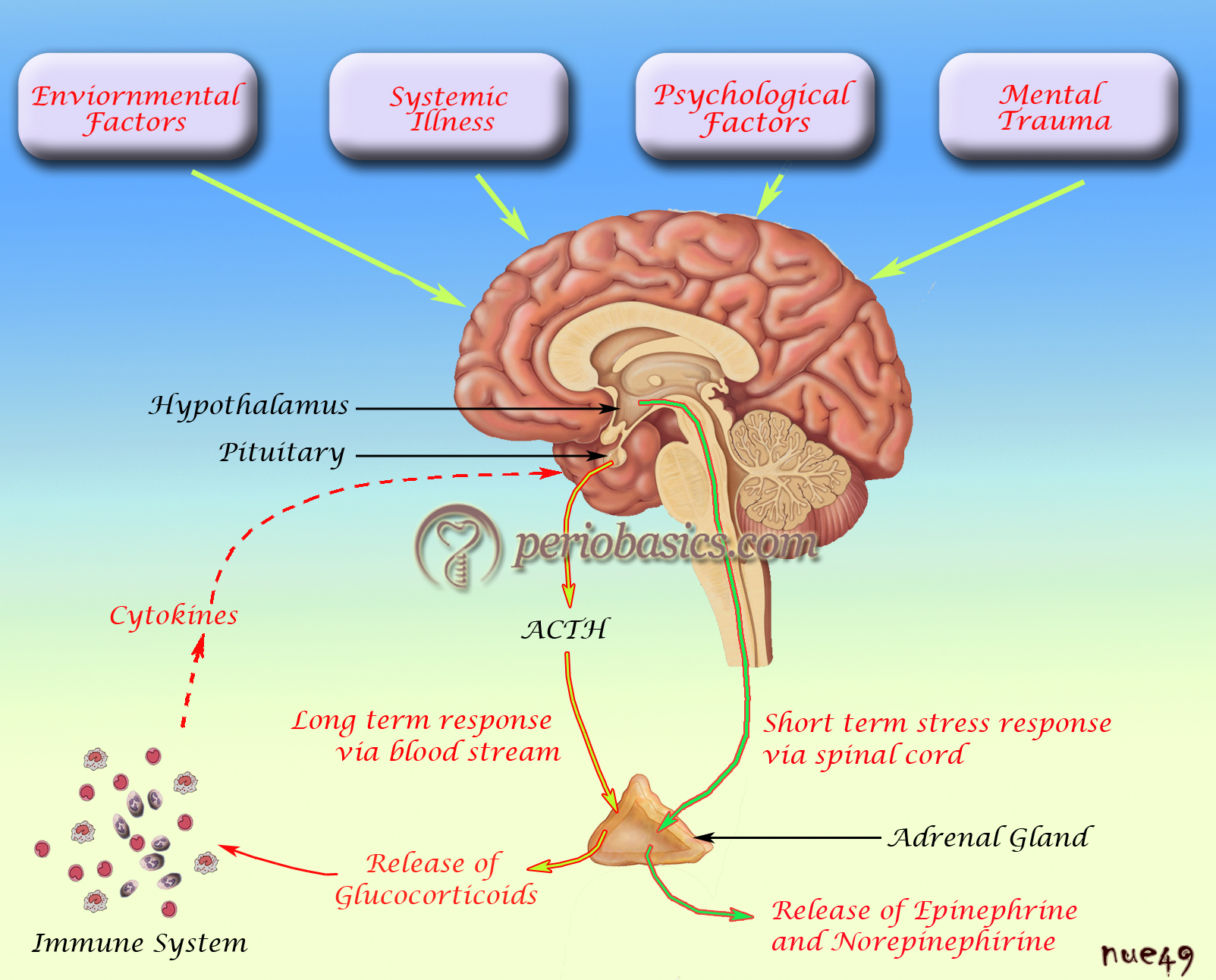
Along with this, the stimulation of autonomous nervous system (ANS) by adrenergic receptors causes the secretion of catecholamines (CAs) (adrenalin/noradrenalin) and chromogranin A (CgA) by the adrenal medulla and sensory nerve fibers. Catecholamines alter the immune response, whereas chromogranin A (CgA) has antimicrobial properties. The interaction of catecholamines with adrenergic receptors results in various cardiovascular and metabolic changes in the body. It has been observed that acute stress situations, such as parachute jump, result in the mobilization of T-helper lymphocytes [Cluster of differentiation (CD) + T-cells], cytotoxic T-cells (CD8+), and natural killer cells (NK cells) in the circulation, resulting in ………… Contents available in the book……………….. Contents available in the book……………….. Contents available in the book……………….. Contents available in the book………
The release of neuropeptides such as substance P, somatostatin, the endogenous opioid peptides (β-endorphin and enkephalins), vasoactive intestinal peptide (VIP), and nerve growth factor from sensory nerve fibers (neurogenic inflammation) causes modulation of immune system activity and the release of cytokines 36. These nerve fibers are situated close to the blood vessels in the periodontal tissue. It has been demonstrated that long-lasting stress results in a substantial increase in the release of substance P from these fibers, causing an enhanced and imbalanced inflammatory reaction. Neuropeptides primarily control and regulate Th1/Th2 cytokine secretions which are involved in the regulation of the immune response. Thus, stress may disturb a regulated immune response, resulting in reduced effectiveness of the response 37.
Effects of stress on host response and other factors
Changes in the production of cytokines and other chemical mediators:
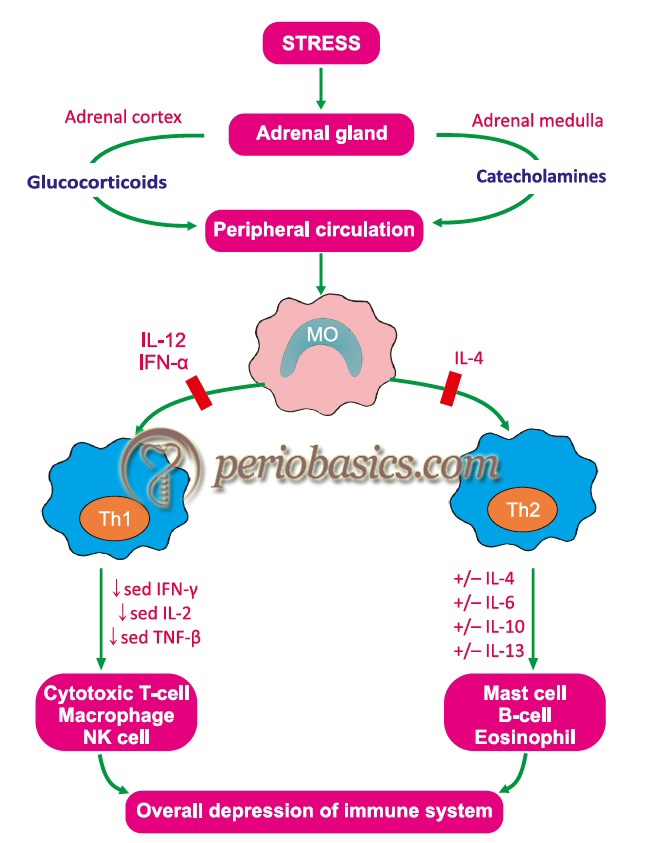
Changes in the cytokine production are observed in stress-related conditions. Interferon-γ and IL-2 produced by Th1 helper cells are suppressed by glucocorticoids, whereas production of IL-4 and IL-10 by Th2 cells remains unchanged. It leads to the suppression of cell-mediated immunity 38. Under the influence of glucocorticoids, production of pro-inflammatory cytokines (IL-6, IL-1, and TNF-α) by monocytes and macrophages is decreased, whereas anti-inflammatory cytokines remain unaffected or are even stimulated 39. Glucocorticoids inhibit arachidonic acid-derived ………… Contents available in the book……………….. Contents available in the book……………….. Contents available in the book……………….. Contents available in the book………
From the above discussion, it is clear that glucocorticoids such as, cortisol, have major suppressive actions on immune and inflammatory responses, resulting in an increased risk for periodontal disease progression.
Cytokine feedback and its effects on HPA axis:
The cytokines produced by the action of various mediators during stress can also activate the HPA axis. It has been demonstrated that peripherally generated cytokines activate the HPA axis at all of its levels, including hypothalamic CRH neuron, pituitary corticotrophs, as well as the adrenal cortex 42-45. The mediators that can activate the HPA axis include lymphocyte-derived γ-Interferon, IL-2, IL-6, macrophage-derived IL-1, and TNF.
So, catecholamines, glucocorticoids and pro-inflammatory cytokines are considered among the principal messengers responsible for the bi-directional communication between the central nervous system and the immune system 46.
Effects of stress on humoral immunity:
IgA and IgG are major antibodies involved in the protection against periodontal disease progression. Glucocorticoids downregulate the synthesis of IgA and IgG and also affect the functions of neutrophils, which may be important in protection against infection by periodontal microorganisms. IgA is a secretory antibody which is important during initial colonization of bacteria. IgG antibodies provide protection by opsonizing periodontal microorganisms for phagocytosis and killing by neutrophils.
Behavioral changes due to mental stress:
Many changes occurring during stress have been proposed to cause periodontal destruction. These include behavioral changes affecting oral health like smoking, poor oral hygiene, and poor compliance with dental care. Another behavioral change is overeating, especially a high-fat diet, which then can lead to immunosuppression through increased cortisol production. All these behavioral changes add up to the other factors explained earlier and cause periodontal disease progression.
Effects of stress on wound healing:
During the early stages of wound healing, immunoinflammatory functions are important. IL-8 and proinflammatory cytokines, such as IL-1 and TNF-α are important during initial healing, as they bring about important changes in the area of injury. They protect against infection by enhancing the recruitment and activation of phagocytes in the area of injury. Along with this, cytokines that are released by recruited cells, regulate the ability of fibroblasts and epithelial cells to remodel the damaged tissue. Matrix metalloproteinase (MMP) activity in the healing area, which plays an important role in the connective tissue ………… Contents available in the book……………….. Contents available in the book……………….. Contents available in the book……………….. Contents available in the book………
Periobasics: A Textbook of Periodontics and Implantology
The book is usually delivered within one week anywhere in India and within three weeks anywhere throughout the world.
India Users:
International Users:
Stress and the microbiology of periodontal disease:
It is believed that microorganisms possess the ability to recognize hormones within the host and utilize them to adapt to their surroundings. Based on this concept, it is also possible that the periodontal microflora may change during stress. One investigation was done to determine whether noradrenaline (norepinephrine), and adrenaline (epinephrine), which are released during human stress responses, act as environmental factors to alter the growth of 43 microorganisms found within the subgingival microbial complexes. In this study, it was found that 20 species within the subgingival biofilm significantly grew when inoculation with noradrenalin, and 27 species significantly grew when adrenaline was introduced. It was also found that there was a difference in the growth response within the bacterial species and within and between the microbial complexes 48. In another study, it was found that chronic psychological stress has a marked impact on the localized immune response to P. gingivalis 49. Thus, during stress two potentially synergistic pathways may facilitate microbial growth and virulence, which are down-regulation of host defenses and up-regulation of bacterial pathogenicity.
The periodontal diseases which are closely related to stress are the necrotizing periodontal diseases, e.g. acute necrotizing ulcerative gingivitis (ANUG). It has been demonstrated that two commonly associated bacteria with acute necrotizing periodontal diseases, Fusobacterium nucleatum subsp. vincentii and Prevotella intermedia have increased growth in the presence of adrenaline (increased in stress) 48.
Stress and grade C (aggressive) periodontitis:
Research has demonstrated a positive correlation between stress and periodontitis with rapid rate of progression. Page et al. (1983) 50 described aggressive periodontitis as a particular disease and established the link existing between aggressive periodontitis and psychosocial factors and loss of appetite. Monteiro da Silva et al. (1996) 51 studied the association of stress with periodontal disease progression by comparing 3 groups: 50 patients with rapidly progressive periodontitis, 50 patients with chronic adult periodontitis, and 50 patients without significant periodontal destruction (controls). The results of the study demonstrated that two psychosocial factors, depression, and loneliness, were significant in distinguishing between groups. The rapidly progressive periodontitis group presented significantly increased depression and loneliness as compared to the chronic adult periodontitis and control groups. In a study done by Kamma et al. (2003) 52 on 25 subjects, it was demonstrated that those subjects who were suffering from aggressive periodontitis were more distressed as compared to subjects suffering from chronic periodontitis. Furthermore, stress was also proposed as a predictive factor for the future loss of clinical attachment.
Stress and acute necrotizing ulcerative periodontal diseases:
Stress is a common factor associated with the development of acute necrotizing ulcerative periodontal diseases. Loesche et al. (1982) 53 reported that increased corticosteroid levels associated with stress may be a precipitating factor for ANUG. The increased corticosteroid levels enhance bacterial invasion of the interdental region by weakening host inflammatory response, or by inducing relative ischemia in the gingival papillary regions. Furthermore, these changes may act as an important nutritional factor for Bacteroides melaninogenicus, P. intermedia, thus providing these microorganisms with a selective nutrient advantage, with subsequent overgrowth and increased inflammatory response. In a study, Cogen et al. (1983) 54 reported defective leukocyte function in ANUG patients as compared to healthy controls matched for age, sex, race and general plaque accumulation. The authors suggested that stress-induced elevated levels of cortisol in ANUG patients may be responsible for these alterations in leukocyte function.
Effects of stress on salivary flow and components:
It has been reported that stress affects the pH, calcium-pH balance and flow rate of saliva 55. Strongin and Hinsie (1938) 56 have reported that depressed patients have a lower rate of salivary flow, whereas manic patients have a higher rate of salivary flow and more basic pH. In another study, Queiroz et al. (2002) 57 examined the relationship between stress, salivary flow rate and oral volatile sulfur-containing compounds (VSCs) in undergraduate dental students. The results demonstrated ………… Contents available in the book……………….. Contents available in the book……………….. Contents available in the book……………….. Contents available in the book………
Bruxism:
Bruxism is the clinical term for the grinding or clenching of teeth while asleep 58. There is a lot of evidence suggesting a positive correlation between physiological stress and bruxism 59-63. However, some studies did not find any association between bruxism and stress 64, 65. Along with bruxism, individuals suffering from anxiety also often report other oral-related symptoms, including difficulties with chewing/ swallowing food, dry mouth 66 and jaw-related problems 58. All these factors affect the overall progression of periodontal diseases.
Response to periodontal treatment:
The management of stress is an important component of the complete periodontal treatment of the patient. Stress coping strategies should be designed to reduce the stress level of the patient. Genco et al. (1999) 8 in a cross-sectional epidemiological study of 1426 adults, aged 25-74 years, evaluated the relationship between psychosocial stress, coping in response to stress, and periodontal disease. The result of the study demonstrated that psychological stress adversely affects the outcome of periodontal treatment and that the effects of psychosocial stress on the periodontal disease can be modulated by adequate coping behaviors. In another study, Wimmer et al. (2005) 67 demonstrated that patients with maladaptive coping with stress have more advanced disease and poor response to a non-surgical periodontal treatment.
Thus, to achieve adequate results, stress coping stretegies should be adopted while planning treatment for a patient with periodontal disease.
Conclusion
Presently, we have sufficient evidence that stress can act as a significant risk factor in the development of periodontal diseases. Evaluation of the patient’s stress level during diagnosis may help us in determining the prognosis of the periodontal condition. Furthermore, it is likely that systemic diseases such as diabetes, cardiovascular disease, preterm delivery, and osteoporosis may share psychosocial stress as a common risk factor in the progression of periodontal diseases. However, our knowledge regarding effect of stress on various aspects of periodontal health and disease is still limited. Extensive research work is required to fully understand the molecular and cellular basis of the role of stress in periodontal diseases.
References
References are available in the hard-copy of the website.

